Triage AI

Developing a Data-Driven Triage
AI Solution for the RCC
👤 Background
The Assistive Technology department at the Rehabilitation Centre for Children (RCC) is struggling with a manual triage process that leaves patients waiting over 100 days for care. Faced with high demand and limited capacity, the team aims to implement a data-driven AI algorithm to automate referral prioritization. They wish to integrate this solution into their current workflow to drastically reduce administrative burden. Ultimately, they are determined to eliminate backlogs and ensure equitable, timely access to therapy for all children.
Identified Solution
❤️ Need

Our proposed In-House AI Triage Algorithm is a data-driven software solution designed for the RCC Assistive Technology department to automate patient referral prioritization.
- It aims to eliminate patient backlogs and reduce wait times by shifting from a manual review process to a dynamic, evidence-based model.
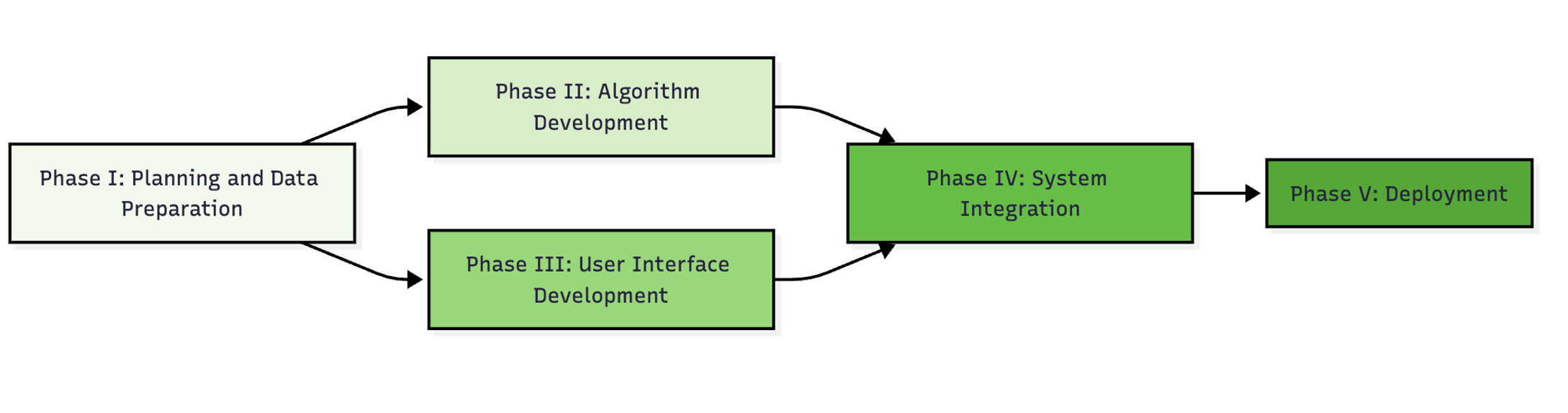
- The system seen in Figure 1 calculates a Priority Index for each referral based on medical complexity and urgency, integrating directly with the current Accuro scheduling system.
Design a data-driven algorithm for the RCC that helps streamline patient scheduling by providing evidence-based priority recommendations. The solution must integrate seamlessly with the existing Accuro software, must strictly comply with PHIPA data privacy regulations, and must allow for immediate clinician override.

🎯Objectives
- Classify referrals into 5 priority levels
- Process 200+ referrals per month
- Generate recommendations in < 5 seconds
- Reduce admin time to < 5 hours/week
- Clinically acceptable vs. expert judgment
🚧 Constraints
- Strict PHIPA & RAID 3 Compliance
- Zero cost for initial software (CDAP Grant)
- Seamless Accuro integration
- Must allow clinician override
🔑 Functions
- Calculates weighted “Priority Index”
- Anonymizes patient data for processing
- Auto-populates waitlist metrics
- Provides audit logs for transparency
🧑 My Individual Contributions
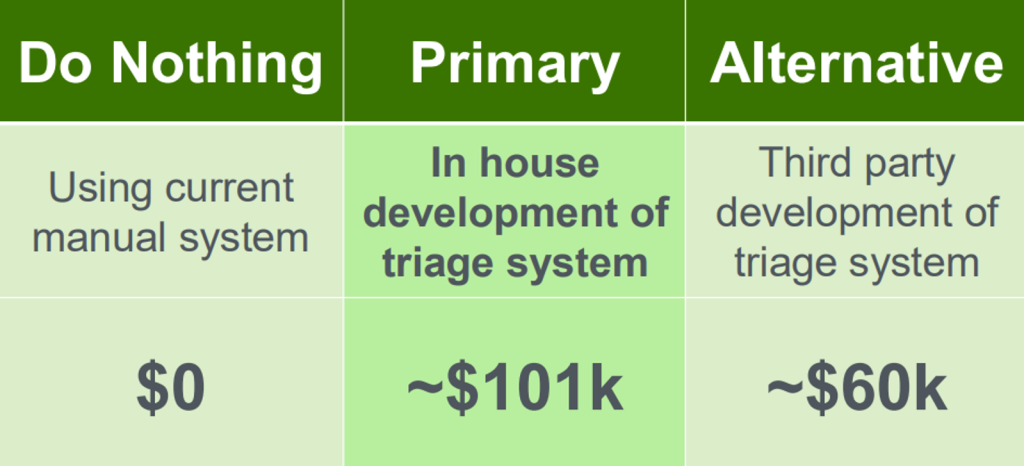
- Conducted the Economic Analysis, calculating Net Present Value (NPV) for both in-house and external options to justify the final recommendation. See Figure 3 for cash flow diagram.
- Developed the Critical Path (Figure 2), identifying zero-slack activities in the 104-week timeline to ensure the project stays on schedule.
- Authored the Executive Summary and Background sections, synthesizing complex clinical bottlenecks into clear problem statements.
- Collaborated with RCC partners (Shea Hunt) over hemail to define technical constraints regarding server space (10U) and data privacy (RAID 3).
🔨 Applied Skills
🧠 Soft Skills
- Stakeholder Management
- Strategic Planning
- Technical Writing
- Ethical Reasoning
⚙️ Hard Skills
- Net Present Value (NPV)
- Critical Path Method (CPM)
- Data Governance
- Feasibility Analysis

📐 Decision Process/Analysis
1. We analyzed the triage bottleneck (10 hours/week lost) and identified the need for a data-driven solution.
2. We compared two distinct paths: Labour-Intensive (In-house) vs. Capital-Intensive (External Contractors).
3. Economic Analysis was performed using an 8% MARR. Option 1 yielded an NPV of $101,005 vs Option 2’s $60,778.
4. We identified that In-house development reduces the risk of the system being reliant on external contractors.
5. A 104-week Critical Path was designed to accommodate the limited engineer availability (1-2 hours/week).
6. The final decision prioritizes capacity building within the RCC over speed of deployment.
- ❌ The External Approach offered speed (1 year) but required $40k upfront and created “vendor lock-in.”
- ✅ We selected In-House Development to retain IP, reduce variable costs, and ensure the algorithm adapts to changing clinical needs.
- ❌ Do-Nothing approach had $0 investment but resulted in continued patient backlog and staff burnout.
- ✅ The AI Solution reduces wait times from median 60 days to <30 days, improving patient quality of life.
Srategic Considerations
Economic Feasibility
- Leverages CDAP Grant ($15k) and RCC seed funding ($10k) to offset initial server setup.
- Relies on “sunk cost” of existing engineering salaries rather than new expenditures.
Clinical Adoption
- Deep involvement of clinical leads prevents the technology from being abandoned and better understood by those maintaining it.
- Transparent “Priority Index” ensures clinicians trust the AI’s recommendations and are also able to manually override.
Scalability
- Potential to package and sell the algorithm to other pediatric centers (Revenue stream).
- Economies of scale achieved by expanding to other RCC / government departments with negligible marginal cost.
Final Recommendation
The In-House Strategy
- The team recommends the Labour-Intensive (In-House) action plan, spanning 104 weeks.
- It delivers a superior NPV of $101,005 and ensures the solution is tailored to the RCC’s unique Accuro workflow.
- While slower than hiring external contractors, this approach builds internal capacity and eliminates the risk of reliance on outside vendors for future updates.
Personal Reflective Summary
Being the only virtual student changed how I approached this project. I wasn’t able to interact with my teammates in person or walk up to the TAs for quick questions. Instead, I had to be intentional about reaching out. Living in Calgary put me two hours behind the team in Ontario, which required sacrifice, but my group was accommodating. While being there in person would have made communication easier, being remote forced me to be extra clear to ensure we didn’t miss anything.
A specific challenge happened during a meeting with our partners, Nicole and Shea. The team had the laptop facing away, so they couldn’t see me trying to ask a question about security. The meeting ended without my input. I decided to email Shea immediately after to ask my questions. This turned out to be critical. His reply revealed specific PHIPA guidelines we were missing. If I hadn’t taken the initiative to send that email, we would have delivered a solution that was legally non-compliant and not considering in-house data servers.
Now coming back to our decision between hiring external developers or using internal staff. At first, I wanted the external option because it was faster. But looking back, I realize that there was alot more risk if we went that route. If the RCC spent $40,000 upfront and the software broke two years later, they wouldn’t have the budget to hire the consultants back to fix it. Furthermore for any maintainence or upgrades we would have to rehire external contractors which would be costly. By choosing the slower, in-house option, we ensured the RCC could maintain the system themselves. Looking past just the cost, I learned that the best solution isn’t always the fastest one. It is the one the client can actually afford to keep running.